 Briefing
Briefing
COVID-19 – End of the Public Health Emergency – Impact on Employer Sponsored Health Plans
On January 30, 2023, the Biden administration announced that it will end both the national emergency and public health emergency COVID-19-related declarations that have been in effect since 2020. While this most recent announcement was not a formal declaration, employers and plan sponsors should plan for both declarations to end, as announced, on May 11, 2023.
National COVID-19 Emergency and the “Outbreak Period”
In 2020, the U.S. Department of Labor’s Employee Benefits Security Administration (EBSA) and the Internal Revenue Service (IRS) issued regulatory guidance extending certain timeframes impacting group health plans during the COVID-19 national emergency. That guidance established a period of time from March 1, 2020 until 60 days after the announced end of the COVID-19 national emergency (or such other date announced by EBSA and the IRS in later guidance) as the “Outbreak Period.”
Group health plans were instructed to disregard the Outbreak Period for purposes of:
- The 30-day period to request a special enrollment in a group health plan;
- The 60-day period to request enrollment into a group health plan upon losing eligibility for CHIP coverage becoming eligible for the CHIP subsidy;
- The date within which individuals may file a benefit claim under a plan’s claims procedures;
- The date within which a claimant may file an appeal of an adverse benefit determination under a plan’s claims procedures;
- The date within which a claimant may file a request for an external review after receipt of an adverse benefit determination or final internal adverse benefit determination;
- The date within which a claimant may file information to perfect a request for external review upon a finding that the request was not complete;
- The 60-day election period for COBRA continuation coverage;
- The date for making COBRA premium payments; and
- The date for a group health plan, sponsor, or administrator to provide a COBRA election notice.
In February of 2021, EBSA and the IRS released additional guidance in Disaster Relief Notice 2021-01, which stated that "individuals and plans with timeframes that are subject to the relief under the Notices will have the applicable periods under the Notices disregarded until the earlier of (a) 1 year from the date they were first eligible for relief, or (b) 60 days after the announced end of the National Emergency (the end of the Outbreak Period). On the applicable date, the timeframes for individuals and plans with periods that were previously disregarded under the Notices will resume. In no case will a disregarded period exceed 1 year."
On February 18, 2022, President Biden issued a notice extending the COVID-19 national emergency through March 1, 2023. In its January 30, 2023 announcement, the administration stated that the National Emergency would be extended one final time and expire on May 11, 2023.
Impact
With respect to the Outbreak Period, this means that the clock will still run for one year from the date an individual was first eligible for relief, but all Outbreak Period relief will end as of July 10, 2023 (60 days after the May 11 expiration date.)
Practice Tip: If you think about July 11, 2022 as a “turning point,” events and deadlines prior to that day will enjoy a one-year extension to the deadline/timeline that would otherwise apply. If the event/deadline occurs after July 11, 2022, they will not get the full year. They’ll get the lesser of the end of the outbreak period plus their standard timing (30 days, 60 days, as applicable).
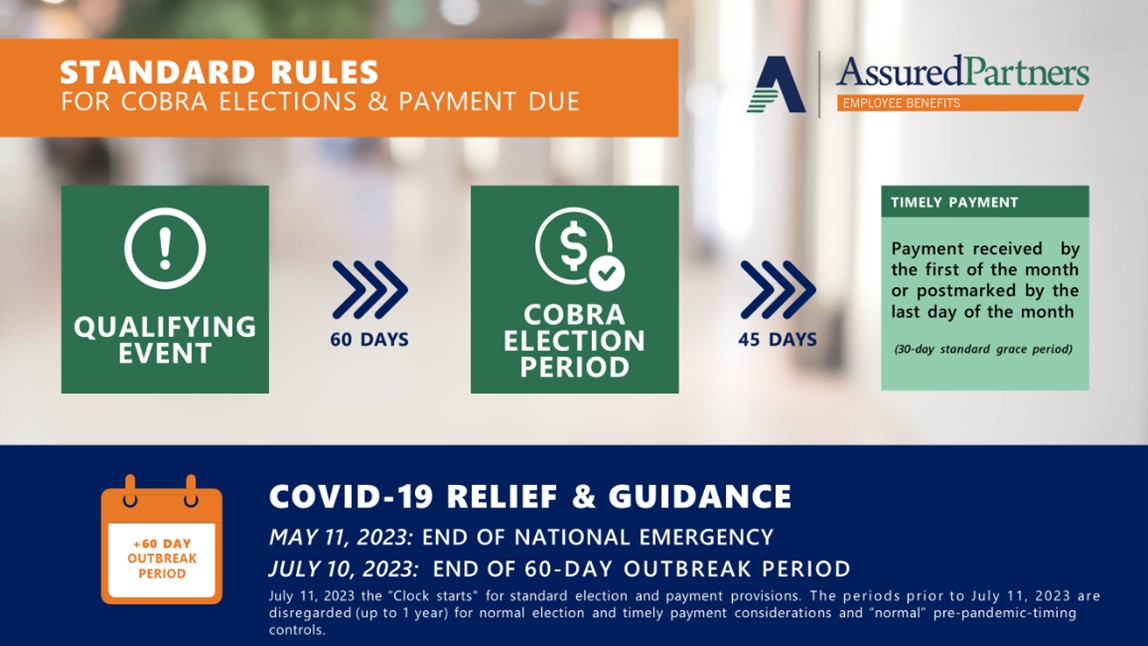
- Deadlines and grace periods that would have otherwise begun on or before July 10, 2022 will enjoy a full one-year extension to their deadline or grace period.
- Example 1: Plan A normally provides 60 days from the date of their COBRA Election Notice to elect COBRA. Fred’s COBRA Election Notice was dated Apr. 15, 2022. Under the Outbreak Period, Fred’s 60-day COBRA election window is tolled from April 15, 2022 through April 14, 2023, and his 60-day election period runs through June 13, 2023 (60 days from April 14, 2023).
- Deadlines and grace periods that would have otherwise begun on or after July 11, 2022 will not get a full-year extension. Instead, their grace period or window to act will begin July 11, 2023.
- Example 1: Same as the first example above, but Fred’s COBRA Election Notice was dated Nov. 8, 2022. Fred’s 60-day period to elect COBRA was tolled until July 10, 2023 (the last day of the Outbreak Period), and his 60-day election period runs through Sep. 8, 2023 (60 days from July 10, 2023).
- Example 2: Same as the second example, above, but Wilma’s plan must disregard the period ending July 10, 2023, which would mean Wilma’s deadline to enroll Pebbles would be August 9, 2023 (30 days from the Outbreak Period’s July 10, 2023 end date).
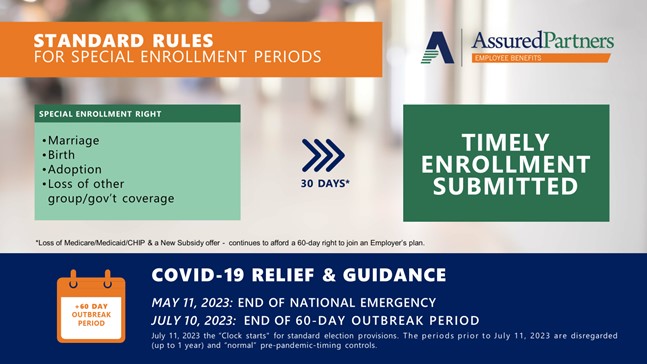
Note that while the tolling (deadline extensions) apply to HIPAA Life Events (birth, adoption, placement for adoption, marriage, divorce, death of an employee, etc.) they do not apply to the other (optional) Section 125 mid-year election change reasons (e.g., significant cost changes, the spouse’s Open Enrollment, etc.).
Finally, as the administration works to formalize the end of the Outbreak Period, it may issue additional guidance that could alter the current understanding of how this all will work. We will continue to provide updates as additional guidance warrants.
COVID-19 Public Health Emergency
The declaration of a public health emergency, first made in January of 2020, was most recently renewed by the administration on January 11, 2023. While under the current declaration it is set to expire on April 11, 2023, the administration plans to extend the Public Health Emergency one additional time to May 11, 2023.
Impact
On May 11, 2023, the following federal requirements for group health plans will expire (however when each carrier or claims-paying TPA will choose to implement that change is to be determined):
- Coverage of COVID-19 diagnostic testing and related services (including tests administered by providers and over-the-counter tests) without cost-sharing, prior authorization, or other medical management requirements.
- Coverage of COVID-19 vaccines—including booster doses—from out-of-network providers without cost-sharing, prior authorization, or other medical management requirements. In-network COVID-19 vaccinations will remain free as preventive services under the ACA as well as other federal laws.
- The ability to offer stand-alone telehealth benefits and other remote care services to participants who are not eligible for major medical coverage.
- The suspension of enforcement actions under the Mental Health Parity and Addiction Equity Act (MHPAEA) related to the coverage of COVID-19 testing items and services without cost-sharing, prior authorization, or other medical management requirements.
AP Keenan is not a law firm and no opinion, suggestion, or recommendation of the firm or its employees shall constitute legal advice. Clients are advised to consult with their own attorney for a determination of their legal rights, responsibilities, and liabilities, including the interpretation of any statute or regulation, or its application to the clients’ business activities.
Subscribe
Subscribe to the Keenan Blog




